The goal isn’t to chase perfect numbers—it’s to keep cholesterol moving freely through your Alzie’s arteries.
Because when blood flows freely, the brain stays nourished.
The lipid panel shows you how well that flow is happening—and where it’s getting stuck.
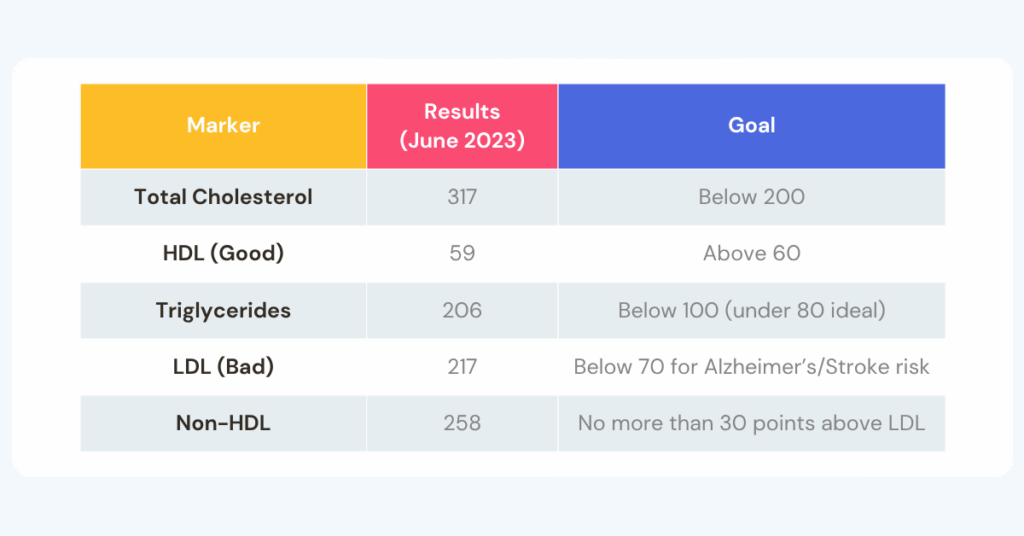
Now let’s unpack what those numbers meant—and how they showed us where to focus.
Total Cholesterol — The Grocery Bill
At first glance, this was the only number anyone talked about.
Her total cholesterol was 317—a number that sounded scary but didn’t tell us much.
Think of total cholesterol like your grocery bill.
It tells you what you spent, but not what you bought.
You can’t tell if that $317 went to fresh produce or junk food.
For the brain, this number matters only when you look at what’s inside it—how much is “good” (HDL), how much is “bad” (LDL), and how much is leftover (Non-HDL).
Goal: Below 200 mg/dL is desirable, but balance matters more than the total.
Fix: Lifestyle. Focus on fiber, balanced meals, and regular movement.
LDL — The Traffic Jam
Once we understood the “bill,” LDL showed us where things were getting stuck.
Her LDL of 217 was the biggest red flag.
Too many LDL particles clog arteries like delivery trucks stuck on narrow streets.
That buildup was quietly starving our mom’s brain of blood, oxygen, and nutrients—the essentials that keep her memories and personality shining through.
Goal: Below 70 mg/dL if you have Alzheimer’s or are genetically at-risk for a stroke.
Fix: Medication + Lifestyle. LDL often needs help from statins, but walking, fiber, and less sugar help the medicine work better.
💡 Caregiver takeaway: When LDL is high, blood isn’t flowing freely—and the brain may not be getting fully “fed.”
Triglycerides — The Sugar Story
After LDL, we turned to triglycerides to understand what was fueling the traffic jam.
Her triglycerides came back at 206.
We’d always thought she was eating healthy. But it turned out, she wasn’t eating wrong—she was eating imbalanced.
Too much sugar hiding in “healthy” foods (flavored yogurt, cereal, fruit juice), and not enough fiber to sweep it out.
That combo fuels insulin resistance, and when the body can’t move sugar efficiently, it stores it as fat in the blood.
That “blood fat” shows up as triglycerides on a lab test—and for our mom’s brain, it meant less steady energy and slower fuel delivery when she needed it most.
Goal: Under 100 mg/dL (below 80 is ideal).
Fix: Lifestyle. More fiber, fewer sweetened foods, and short walks after meals can dramatically lower triglycerides—often within months.
💡 Caregiver takeaway: High triglycerides are your body’s way of saying, “I need more fiber.”
HDL — The Cleanup Crew
Next, we looked at HDL—her body’s cleanup team.
Her HDL was 59, just below the low end of the healthy range.
This is the cholesterol that clears excess fat from the bloodstream.
Think of HDL as the crew that keeps the brain’s highways clear, making sure blood and oxygen can reach every corner.
When HDL runs low, those routes start to clog—and our mom’s brain has to work harder just to stay alert and connected.
Goal: 60 mg/dL or higher—the more, the better.
Higher HDL helps clear cholesterol and keeps blood flowing to the brain.
Fix: Lifestyle. Daily walks, strength training, and healthy fats (such as avocado, olive oil, and nuts) naturally raise HDL.
💡 Caregiver takeaway: High HDL means smoother blood flow—and better-fed brain cells.
Non-HDL — The Leftovers
Finally, we looked at Non-HDL, which shows what’s left after HDL clears it.
Our mom’s number was 258—another sign that her bloodstream was crowded.
When there’s too much leftover cholesterol circulating, it’s harder for blood to move freely through the arteries.
For the brain, that means our mom was getting a slower delivery of nutrients and oxygen to the cells that support memory and movement.
It’s like rush-hour traffic on every route leading to the brain’s most important neighborhoods.
Goal: No more than ~30 points higher than LDL.
If LDL’s goal is 70, aim for Non-HDL ≈ 100.
Fix: Both. Lowering LDL with medication and lifestyle adjustments (fiber, less sugar, more movement) brings Non-HDL down too
💡 Caregiver takeaway:
HDL clears the road; Non-HDL shows what’s still stuck in traffic.
When Non-HDL is high, the bloodstream is crowded and the brain can’t get the steady fuel it needs.


We’re not doctors—just caregivers sharing what we’ve learned in plain English.
Use this information to start a better conversation with your Alzie’s doctors and find what works best for your loved one.


